What We Offer
High Quality Ultrasound is Best Performed in All Three Trimesters
In the first trimester, we establish pregnancy due date, count the number of fetuses and whether multiples are fraternal or identical, look for major fetal problems, establish the location of the placenta and use measurement of the nuchal translucency and other structures to alter the a priori risk of chromosomal anomalies such as Down syndrome and dozens of other disorders such as cardiac anomalies. We also use ultrasound as part of the screening panel for pre-eclampsia. In the first trimester, transvaginal ultrasound usually provides greater quality and detail than transabdominally and allows for more of an “anatomy scan” than abdominally.
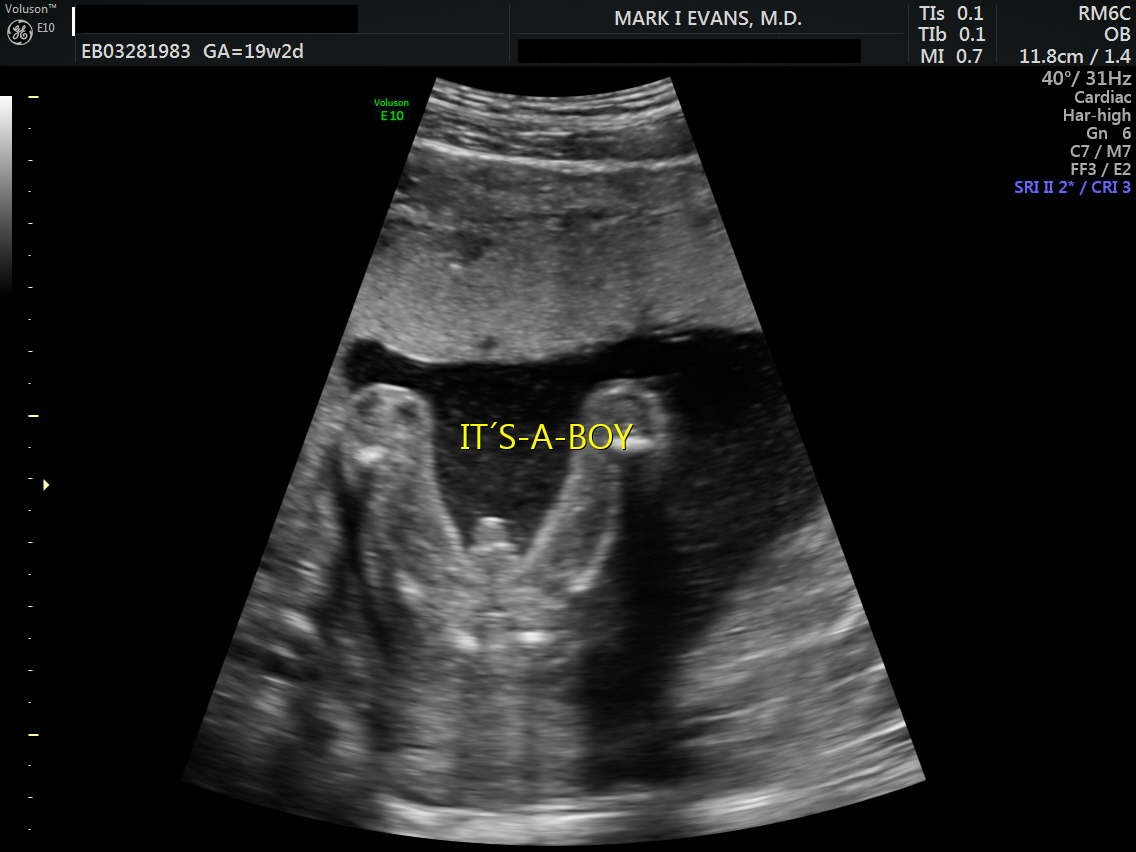
In the second trimester, we do detailed anatomical analysis of the fetus from head to toe. The "anatomy scan" is usually done at about 20 weeks so that there is enough development particularly of the heart and brain for detailed visualization of structures and function. We commonly also perform an “early anatomy” scan at about 16 weeks at which time with increasingly sophisticated equipment, we can find many of the major anomalies. Mostly, this scan provides reassurance that all seems well, but most people would agree that if there is to be an anomaly discovered, it is at least somewhat “less-worse” the earlier we do that.
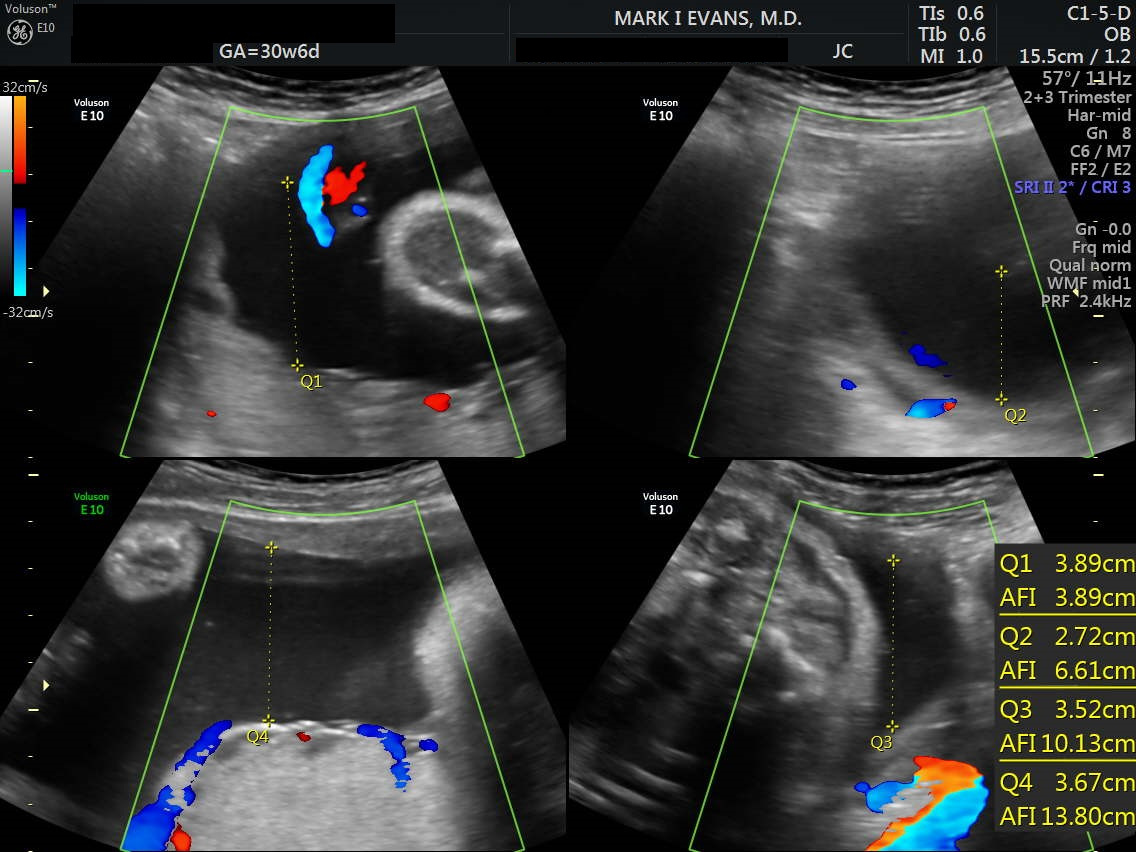
In the third trimester, we follow the rate of growth of the fetus, the proportion of fetal structures, amniotic fluid volume, and placental function. In addition to growth per se, we perform biophysical profiles which are very good predictors of placental function and fetal health. We are very obsessive-compulsive about getting such data - more so than many centers - because we want to know about developing problems as early in the process as possible so that appropriate management can be undertaken before the issues become damaging.
First Trimester Ultrasound, Nuchal Translucency and First Trimester Instant Risk Assessment
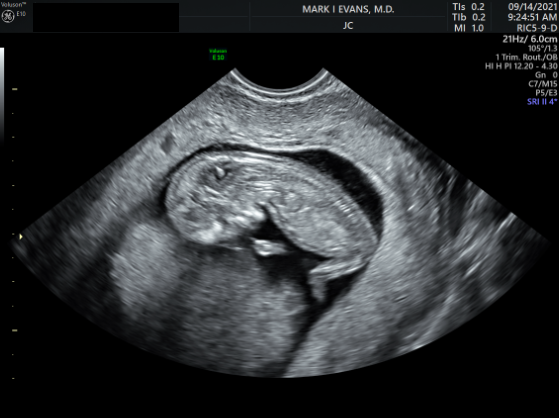
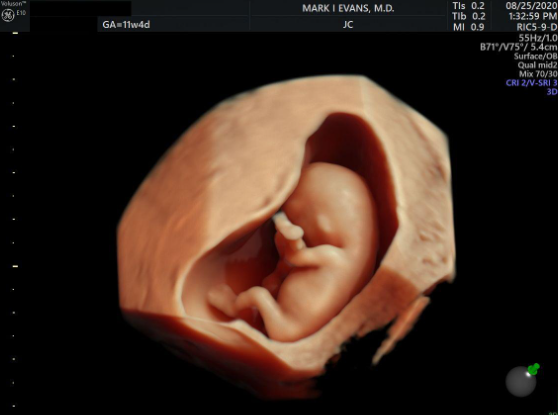
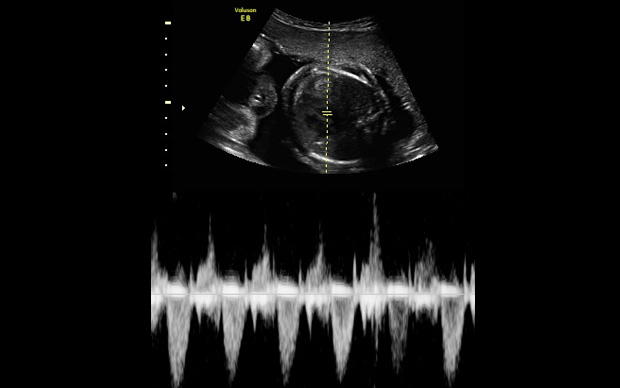
Ultrasound imaging looks at the fetus. First-trimester ultrasound is the most reliable way of establishing the "due date" of pregnancy; of determining the number of fetuses, and whether multiple fetuses are identical or fraternal; and of screening for elevated risk of genetic abnormalities, including Down syndrome and some cardiac, neural, and limb abnormalities.
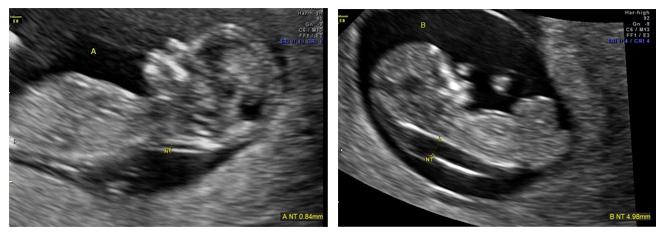
During ultrasound, the crown- rump length (from head to butt) is the most accurate ultrasound assessment for gestational age and due date. The nuchal translucency (NT) (the thickness of the back of the fetal neck) is a non-specific but very important indicator of the presence of multiple anomalies in the fetus. For over 25 years in millions of pregnancies, NT and blood studies for free β hCG and PAPP-A have been shown to be very reliable indicators of many genetic risks that can then be investigated with diagnostic tests (CVS and amniocentesis). The biochemical tests are far cheaper than NIPT, and many governmental and managed care programs will only pay for them and not NIPT.
First-trimester screening results usually either increase or decrease the age-related risk of the pregnant woman for Trisomy 21 (Down syndrome), Trisomy 13, and Trisomy 18. For example, the results may describe a 26-year-old woman as having the risk of carrying a fetus with Down syndrome equivalent to that of a 40-year-old (or vice versa). By performing first-trimester combined screening (free β hCG, PAPP-A, and nuchal translucency ultrasound) about 80% of pregnancies with Down syndrome can be identified in the first trimester. (The second trimester quadruple blood screen can only detect about 80% of cases.) Patients can then use this information to decide whether they wish to have definitive testing, such as CVS, to obtain a specific diagnosis in the first trimester.
First-trimester screening is more sensitive than that in the second trimester or than using maternal age alone. Also, early screening allows early diagnosis of fetal abnormalities, giving parents more time to exercise treatment and management options. It also provides PRIVACY for patients considering serious disorders.
The goal of screening is to maximize the chance of finding a problem that might be there while at the same time minimizing the number of women who require diagnostic (definitive) testing to be certain. For patients having serum screening, patients have a finger stick blood sample taken at 9-11 weeks. Then, at 11-and-a-half to 13 weeks 6 days, we perform the first trimester ultrasound and measure the thickness of the back of the neck—referred to as the Nuchal Translucency (NT) measurement. Accurate measurement of the NT is critical, as its results are used in a formula combined with the gestational age of the fetus (as measured by its length), the age of the mother, and the results of the hCG and PAPP-A blood tests. While the patient is in our office having the US, we can instantly compute the adjusted risk. Low-risk patients can be re-assured and higher risk patients can be offered diagnostic testing via CVS, which provides a definitive answer and can usually be performed at the same visit.
It is important for all patients to remember, however, that screening results do not give a definitive answer but merely alter odds. Whatever the Down syndrome risk may be on screening, the risk of other issues such as sex chromosome abnormalities, rings, translocations, and inversions (on the basis of a karyotype) can be made no lower than about 1/500. Now that microarrays are routinely available for our patients, that minimal number is actually at least 1 100 (which is comparable numerically to what we have been counseling 38 year olds for Down syndrome and common trisomies). Therefore, when we counsel patients, we believe that the lowest possible risk internalized by patients in their decision-making process should be 1/100 if the computed Down syndrome risk is reported as lower than that.
Second Trimester Ultrasound
Genetic ultrasound is part of every diagnostic procedure we perform. In the majority of instances, assessment of fetal structure and sometimes function allows for the reassurance of normality. Unfortunately, we also find pregnancies in which there are significant structural abnormalities that can vary from minor to severe to lethal. We use the state of the art machinery that provides the highest resolution in 2, 3, and 4 dimensions.


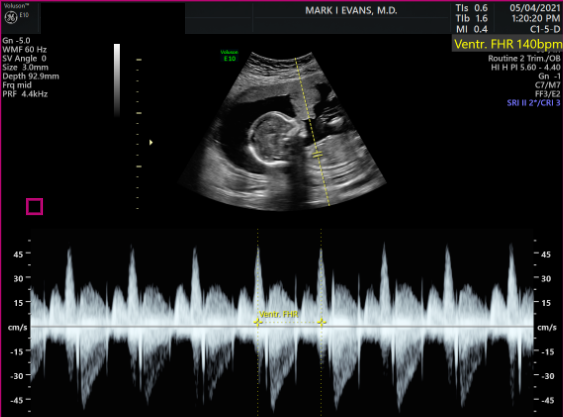
Four Chambers

Profile Image
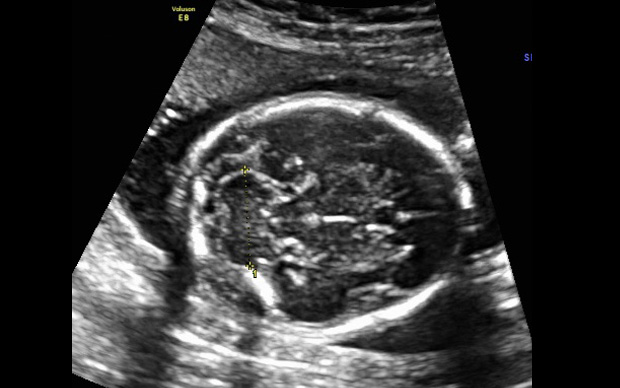
2nd Trimester Brain Structures
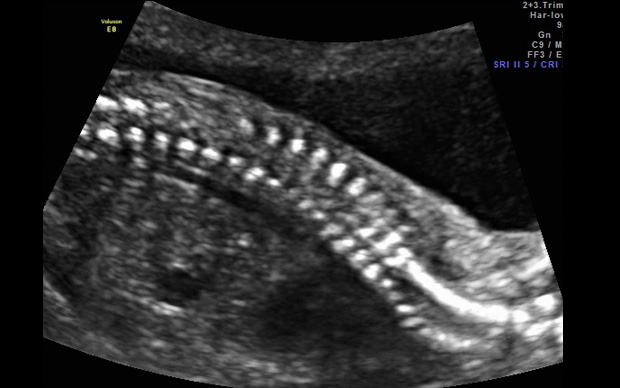
2nd Trimester Spine

2nd Trimester facial 3D
Third Trimester Ultrasound
Third trimester ultrasounds have 2 purposes: 1. To assess fetal growth, and 2. Assess fetal well-being.
Evaluation of fetal growth is best performed in all three trimesters to assure continued, appropriate growth. Further evaluation of fetal health can be obtained by biophysical profiles that document amniotic fluid volume, fetal movement, breathing, and tone. A separate "non stress test" by electronic fetal monitoring at the hospital is often added. Philosophically, we like "data" and are much more aggressive in getting hard data from ultrasounds than do many programs. Earlier appreciation of emerging risks allows for safer, often less dramatic interventions to produce better fetal/neonatal outcomes that might not have been possible with a more laid-back approach.



Pre Eclampsia
Pre-eclampsia (PE) is a disorder of pregnancy. It is not genetic and is most common in first pregnancies or women having their first pregnancy with a new partner. However, all pregnancies are at risk. We were among the first centers in the United States to implement this screening.
Its manifestations include high blood pressure, protein in the urine, and edema. It can progress to eclampsia in which seizures develop, and in the past, eclampsia carried substantial mortality risks to both fetus and mother. Fortunately, with proper recognition and treatment which usually includes delivery of the baby regardless of gestational age, outcomes for both mothers and babies have improved substantially. However, PE can still force the delivery even if very premature. It is for the very premature babies, that the risks are severe.
The cause of PE has been a source of debate literally for centuries. While we now have a much better understanding of how it progresses, there is still no clear “cause.”
Fortunately, we now have available a screening test which has been shown to identify 90% of the early, high-risk cases (i.e. delivery before 28 weeks). For those patients who are identified on time (testing window 11-13.6 weeks) we can initiate therapy with baby aspirin before 16 weeks which lowers the occurrence by 80%. Published data suggest such screening is a highly effective, highly leveraged public health maneuver.
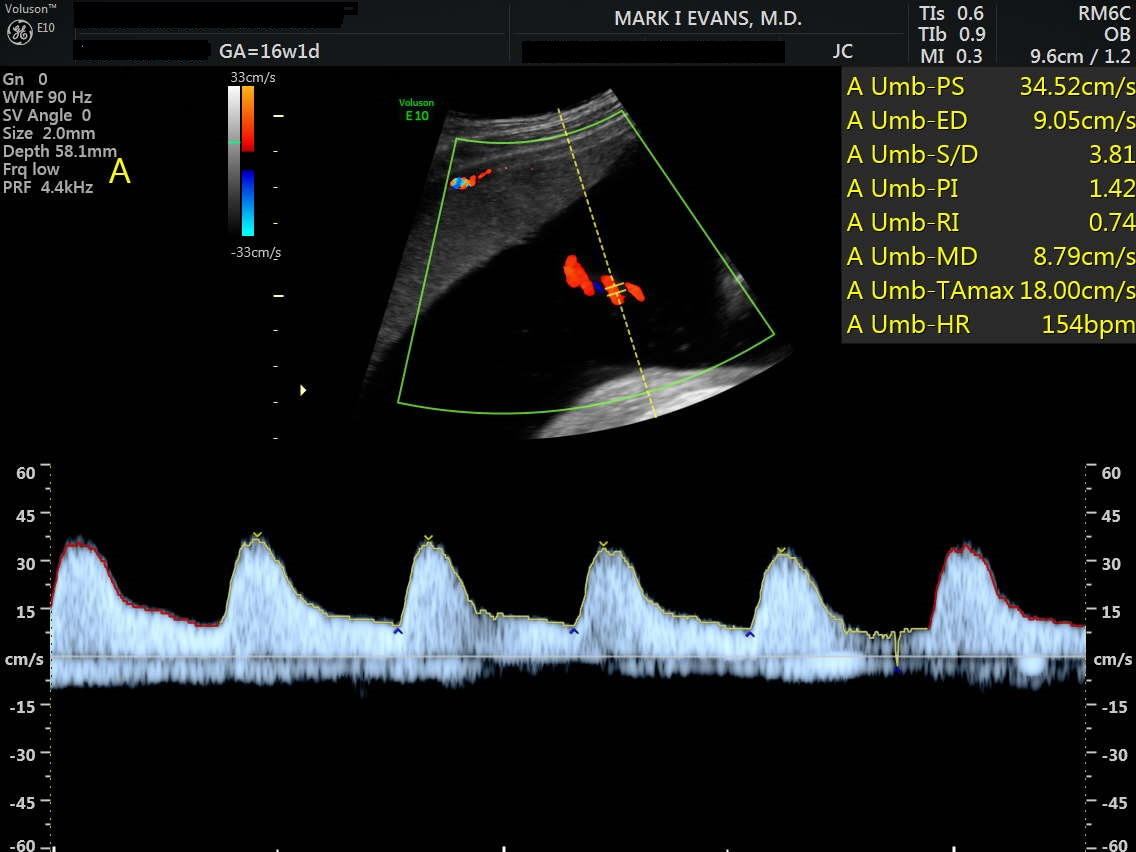
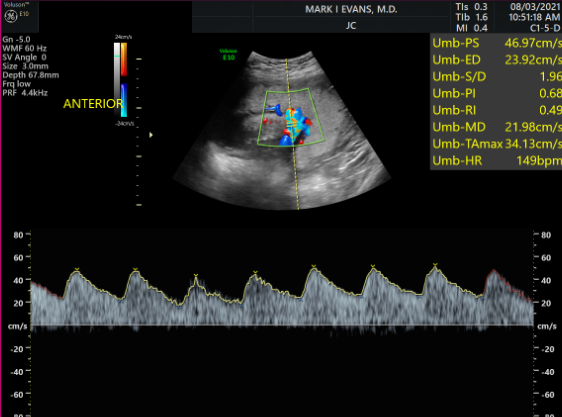
The screening process includes measurement of “mean arterial blood pressure” (both arms), measurement of maternal uterine artery pulsatile index on both sides of the uterus (by ultrasound), and blood testing for PAPP-A and PLGF. PE testing is done at the same time as combined screening (nuchal translucency, free β hCG, and the PAPP-A).
Subnavigation
Evans Pioneer Award Lecture
-
Quick Contact Info
Dr. Mark I. Evans (MD PLLC)
Phone: 212.288.1422
Fax: 212.879.2606
Email: Evans@CompreGen.com
131 E 65TH ST
NEW YORK NY 10065

